Scientists just discovered something that changes everything we thought we knew about depression—and it could save your life.
You walk into your doctor’s office feeling like you’re drowning. Your mind feels foggy. Getting out of bed is a Herculean task. You’ve tried Zoloft. You’ve tried therapy. Maybe you’ve tried both together.
Nothing’s working. Your doctor says, “Let’s try Lexapro this time.” Sound familiar? Here’s the thing that’ll blow your mind: You’ve been getting treated for the wrong disease this entire time.
The $1 Trillion Mistake We’ve All Been Making

What if I told you that depression isn’t actually one condition?
What if it’s actually six completely different diseases that just happen to make you feel terrible in similar ways?
Stanford researchers just proved exactly that. And they didn’t stop there—they figured out how to match the right treatment to the right type of depression.
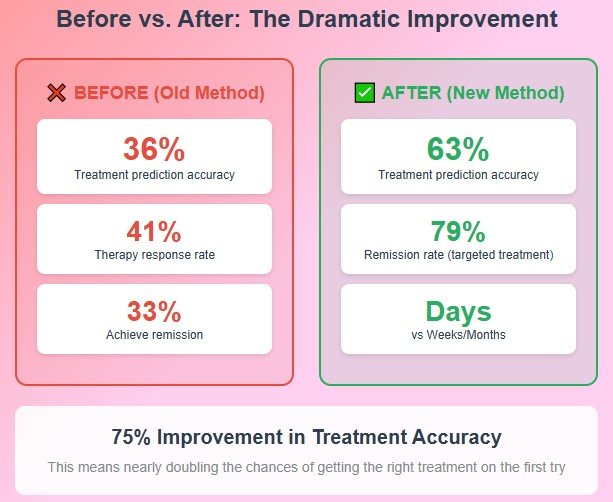
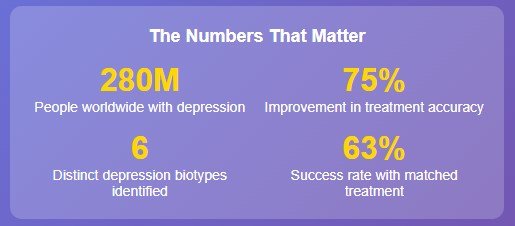
The results? Treatment success rates nearly doubled.
Let me put this in perspective:
- Before: Doctors had a 36% chance of picking the right treatment for you
- After: They now have a 63% chance
That’s like going from flipping a coin to having a crystal ball.
Meet the Woman Who Cracked the Code

Dr. Leanne Williams isn’t your typical researcher.
In 2015, she lost her partner, Jack, to suicide after he battled depression for decades. That loss became her mission—to figure out why depression treatment fails so many people.
Williams heads Stanford Medicine’s Center for Precision Mental Health and Wellness. For the past decade, she’s been asking the question that keeps mental health professionals up at night:
“Why do some people get better with Prozac while others need therapy? And why do we have absolutely no way to predict who needs what?”
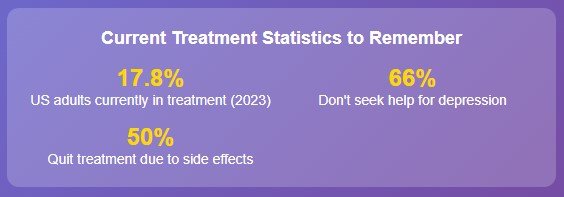
Here’s a stat that should make you angry: 30% of people with depression have “treatment-resistant” depression.
That means multiple medications and therapies have failed them. We’re talking about 2.4 million Americans playing Russian roulette with their mental health.
The Brain Scan That Changes Everything
htmlHow the Stanford Brain Scan Process Works
Step 1: Brain Mapping
Functional MRI scans brain at rest and during cognitive/emotional tasks
Step 2: AI Analysis
Machine learning identifies patterns across 6 brain circuits
Step 3: Treatment Match
Biotype determines optimal medication or therapy approach
Six Brain Circuits Analyzed
Williams and her team did something revolutionary. They took 801 people with depression and anxiety and scanned their brains using functional MRI.
Not just once, twice.
- First, while they were just lying there, doing nothing
- Then, while they performed cognitive and emotional tests
Using artificial intelligence, they found six distinct patterns of brain activity. Six different “biotypes” of depression, each with its own biological fingerprint.
Think about it like this:
If doctors treated all chest pain the same way—whether it was a heart attack, heartburn, or a pulled muscle. That’s exactly what we’ve been doing with depression for decades.
The Six Hidden Types of Depression (And Why This Matters to You)
Type 1: The Overthinker’s Depression

What’s happening in your brain: Overactivity in cognitive regions. What you experience:
- Inability to feel pleasure (anhedonia)
- Trouble making decisions
- Can’t shut off your racing thoughts
- Executive function feels broken
The breakthrough: These people respond best to Venlafaxine (Effexor) compared to other antidepressants.
This type affects more than 25% of people with depression. If this sounds like you and SSRIs haven’t worked, this could be why.
Type 2: The Problem-Solver’s Paradox

What’s happening: Higher brain activity in problem-solving regions. What you experience:
- You’re good at cognitive tasks
- But you mess up executive function tests
- Your brain wants to fix everything
The breakthrough: You respond better to behavioral therapy than medication. Your overactive problem-solving circuits actually help you learn new coping skills faster.
Type 3: The Attention-Deficit Type

What’s happening: Lower activity in attention-control circuits. What you experience:
- Can’t focus during therapy sessions
- Mind wanders constantly
- Struggle to learn new skills
The breakthrough: Talk therapy is less likely to be effective for you. Your brain literally can’t focus enough to benefit from it.
The Mystery Type
Here’s what’s wild: One of the six types showed zero differences in brain activity compared to healthy people.
Williams thinks this means our understanding is still incomplete. There are likely other brain regions involved that we have not yet discovered.
The Numbers That’ll Make You Angry (Then Hopeful)
Let’s talk about what this means in real terms:
The Current Disaster:
- Only 41% of people respond to therapy for depression
- Just 1 in 3 patients actually get better
- 2 out of 3 people with depression don’t even try to get help
- Half of all treatment failures happen because people quit taking their meds
The New Reality:
- 63% accuracy in picking the right treatment (vs 36% before)
- In related Stanford research, 79% of severe depression patients got better with brain-targeted treatment
- Treatment worked in days, not months
Here’s the kicker: Depression and anxiety cost the global economy $1 trillion per year in lost productivity.
When we get treatment wrong, we’re not just failing you—we’re failing everyone.
What This Means for Your Life Right Now

“Okay,” you’re thinking, “this sounds amazing. But when can I actually get one of these brain scans?”
Good news: Stanford has already started using this technology in their new precision mental health clinic.
Better news: Williams says they’re “actively developing the technology for wider use in clinical settings.”
But here’s what you can do TODAY:
If you’ve tried multiple depression treatments without success, don’t give up. This research proves what you’ve probably suspected—your depression really might be different from everyone else’s.
Questions to Ask Your Doctor:
- “Have we considered that my depression might be a different biological type?”
- “What other treatment approaches haven’t we tried?”
- “Are there any clinical trials for precision psychiatry in our area?”
Why This Changes Everything

We’re not just talking about depression here. We’re witnessing the birth of precision psychiatry.
Williams draws a parallel to cardiology: “74 years ago, cardiology lacked imaging tools like MRI or CT scans.”
We’re at the same point with mental health that heart doctors were in the 1950s—right before everything changed.
The same brain circuits involved in depression also control anxiety. This approach could transform treatment for multiple mental health conditions at once.
The Hidden Cost of Getting It Wrong

Here’s what most people don’t realize about depression treatment failure—it’s not just about feeling bad longer.
The ripple effects:
- 40% higher risk of heart disease and diabetes
- Unemployment rates are 60% higher for people with depression
- High schoolers with depression are twice as likely to drop out
- 17.8% of U.S. adults are currently dealing with depression—the highest rate since 2015
Real Talk: What’s Coming Next
htmlThe Future of Mental Health: Next 5 Years
2024-2025
Test non-traditional medications
Wider clinical implementation
2025-2027
Remote treatment tracking
Digital biomarker integration
2027-2029
Insurance coverage expansion
Global implementation
🤖 AI Advancement Goals
- • Discover additional biotypes beyond current 6
- • Predict treatment response in 24-48 hours
- • Integrate genetic and lifestyle factors
📊 Research Pipeline
Williams isn’t stopping here. Her team is planning to:
- Test more treatments across all six biotypes
- Use AI to discover new biotypes we haven’t found yet
- Connect brain scans to smartphone apps for real-time monitoring
Your phone tracks your mental health recovery in real-time, guided by your specific brain scan results. That’s not science fiction. That’s the next 5 years.
The Bottom Line (And Why You Should Care)
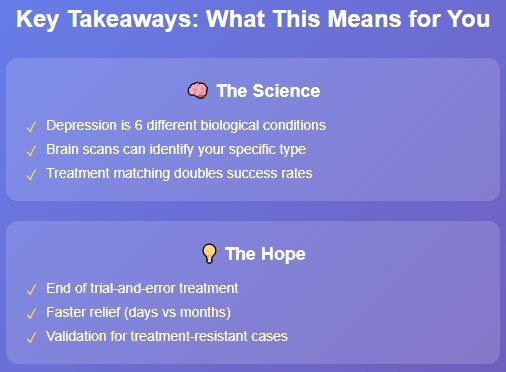
For decades, we’ve been playing mental health roulette.
“Try this antidepressant. If it doesn’t work, we’ll try another one. Maybe some therapy too.”
That era is ending.
We’re moving from “let’s see if this works” to “this should work for your specific brain.”
Think about what that means:
- No more months of waiting to see if a medication works
- No more feeling like you’re broken because treatment #4 didn’t work either
- No more wondering if it’s “all in your head”
Your brain is as unique as your fingerprint. Your treatment should be too.
What You Should Do Right Now
If you’re struggling with depression:
- Don’t give up if previous treatments haven’t worked
- Talk to your doctor about these new findings
- Ask about clinical trials in precision psychiatry
- Share this information with someone who might need it
If you know someone battling depression:
- Forward them this article
- Remind them that treatment failure doesn’t mean they’re a failure
- Let them know that science is finally catching up to what they’ve experienced
The future of mental health treatment isn’t about finding one-size-fits-all solutions. It’s about recognizing that your depression is as unique as you are—and treating it that way.
This research was published in Nature Medicine in June 2024. While this technology isn’t widely available yet, clinical trials are ongoing, and implementation has begun at select medical centers. Always consult with healthcare professionals about your specific situation.
What’s your experience with depression treatment been like? Have you felt like your depression was “different” from others? Share your thoughts in the comments below.






