
What if I told you that your future aches and pains might be predictable… and preventable?
Ever wonder why some people seem to “fall apart” physically after going through tough times?
You know what I’m talking about. Maybe it’s your friend who went through a messy divorce and suddenly can’t get out of bed without her back screaming. Or your coworker who’s been stressed about work for months and now complains about constant headaches.
We usually brush it off as “getting older” or “just stress.”
But what if it’s something much more specific – and much more preventable?
New research from University College London just dropped a bombshell that changes everything we thought we knew about the mind-body connection. And honestly? It’s both terrifying and hopeful at the same time.
The 8-Year Warning You Never Saw Coming
The Depression-to-Pain Timeline
Based on 21-year longitudinal study of 7,336 adults
8 Years Before Pain
Depression symptoms begin subtle climb
Often dismissed as “life stress”
5 Years Before Pain
Mental health decline accelerates
Sleep patterns disrupted
2 Years Before Pain
Loneliness peaks, inflammation rises
Body begins stress response
Physical Pain Begins
Depression symptoms at peak intensity
Both conditions now feed each other
Study Findings
Here’s the part that’ll make you sit up straight:
Depression can predict physical pain up to 8 years before it starts.
Not 8 days. Not 8 weeks. 8 years.
The researchers followed over 3,600 people for more than two decades. What they discovered was like watching a slow-motion car crash in reverse.
People who developed chronic pain had been showing worsening depression symptoms for nearly a decade before their first real ache.
Think about that for a second. Your mind isn’t just connected to your body – it’s literally writing tomorrow’s pain story today.
The Timeline That Nobody Talks About

Here’s how it actually unfolds:
- 8 years out: Depression symptoms start their quiet climb upward
- 5 years out: Mental health continues declining, but you might not notice
- 2 years out: Symptoms accelerate, loneliness increases
- Day zero: Physical pain begins… right when depression peaks
- Years after: Both conditions feed off each other, getting worse together
“Our study shows that depressive symptoms and loneliness worsen long before pain begins,” explains lead researcher Dr. Mikaela Bloomberg.
“This suggests the potential for early mental health support to reduce or delay later pain.“
Translation? Your future doesn’t have to hurt if you pay attention to the warning signs.
Why This Isn’t “Just In Your Head”

Let me guess – you’re thinking this sounds like psychological mumbo-jumbo, right?
Wrong.
This is hardcore biology. And it’s happening in your brain right now.
Your Brain’s Downtown District

Your brain is like a busy city. Pain and depression? They both set up shop in the same downtown district.
This neighborhood includes:
- Your prefrontal cortex (decision-making center)
- The hippocampus (memory headquarters)
- Your amygdala (fear and emotion processing)
- The anterior cingulate (where emotions meet pain)
When depression moves in and starts making noise, physical pain can’t help but be affected. They’re literally neighbors sharing walls.
The Inflammation Highway
But here’s where it gets really wild.
Depression doesn’t just share brain space with pain. It actively creates the biological conditions for pain to thrive.
Here’s what happens inside your body:
Your depressed brain starts sending out chemical distress signals called cytokines. These are supposed to help you heal from injury.
But when depression keeps these signals firing without an actual wound to heal? Your body gets confused.
It’s like having a smoke alarm that goes off every day for years. Eventually, it doesn’t just annoy you – it damages the house.
The result? Chronic inflammation can literally rewire your pain pathways and make you hypersensitive to physical discomfort.
The Numbers That’ll Make You Think Twice
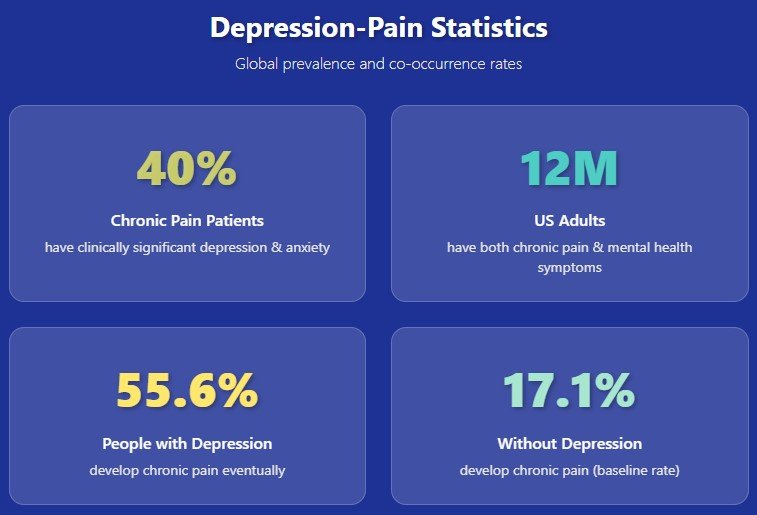
Still think this only affects a few unlucky people?
Think again.

- 40% of people with chronic pain also have clinically significant depression or anxiety
- 12 million Americans right now have both chronic pain and mental health symptoms
- 55.6% of people with anxiety/depression eventually develop chronic pain
- Only 17.1% of people without mental health issues develop chronic pain
The math is pretty clear: Your mental health today is one of the strongest predictors of your physical health tomorrow.
Where Depression Shows Up in Your Body

Want to know something fascinating?
The UCL study revealed exactly where depression tends to “land” when it becomes physical pain.
The top targets:
- Lower back (35% of people)
- Knees (25% of people)
- Hips (20% of people)
- Feet (15% of people)
Notice a pattern? These are all weight-bearing parts of your body – the joints and muscles that literally carry you through life.
When emotional stress converts to inflammation, it targets the parts of you that are already working the hardest.
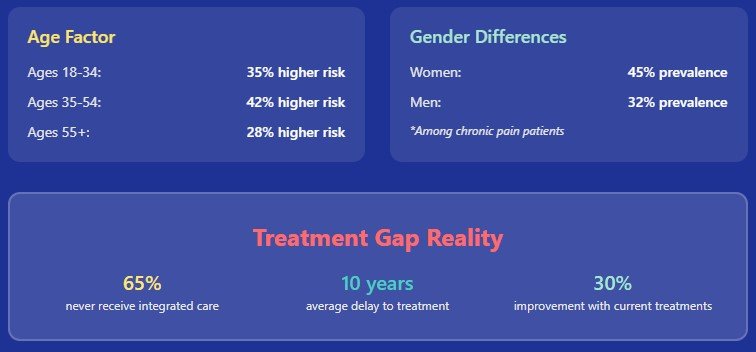
The Social Connection Surprise
Loneliness vs Social Isolation
Quality relationships matter more than quantity
Loneliness
Subjective feeling
Definition:
Feeling disconnected even when people are around you
Pain Connection:
Strong predictor – increases before and after pain onset
Social Isolation
Objective measure
Definition:
Actually being alone, lack of social contacts
Pain Connection:
No significant difference between pain and non-pain groups
Research Findings
Loneliness Timeline
- Increases 5+ years before pain
- Peaks when pain begins
- Remains high after pain onset
- Follows same pattern as depression
Social Isolation Pattern
- Remains relatively constant
- No significant pre-pain increase
- Little difference between groups
- Quantity doesn’t predict pain
The Social Connection Spectrum
❌ What Doesn’t Protect
✅ What Actually Protects
Key Insight: You can be surrounded by people and still feel lonely. It’s the quality of your connections, not the quantity, that protects against future pain.
Here’s a plot twist nobody saw coming.
The study found that loneliness followed the same troubling pattern as depression. It increased for years before pain started and stayed high afterward.
But here’s the kicker: social isolation didn’t follow the same pattern.
What’s the difference?
- Loneliness = feeling disconnected even when people are around
- Social isolation = actually being alone
The takeaway? Having 500 Instagram followers won’t protect you from pain. But having one person who truly gets you? That might.
Quality beats quantity every single time.
The Money Factor Nobody Wants to Talk About
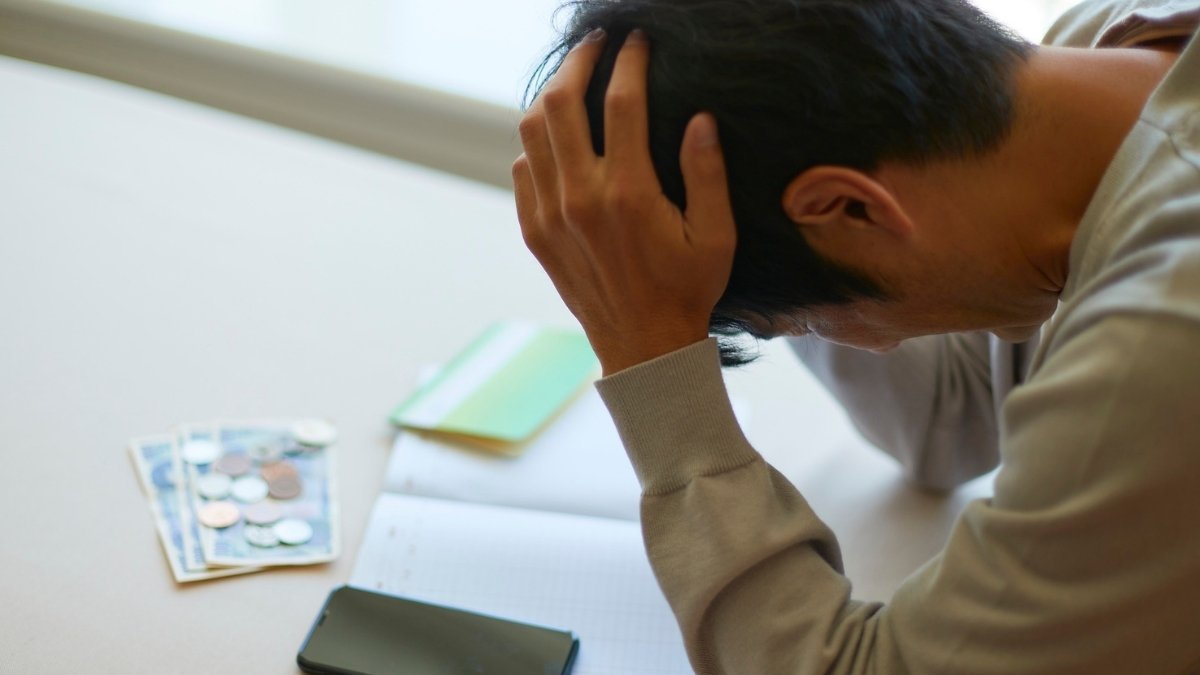
Ready for some uncomfortable truth?
The depression-to-pain pipeline moves faster if you’re struggling financially.
People with less education and wealth showed:
- Steeper increases in depression symptoms
- Faster progression to physical pain
- Worse outcomes overall
Why? It’s not just about healthcare access (though that matters). When you’re already stretched thin, you have fewer resources to:
- Take time for mental health care
- Manage stress effectively
- Build strong support networks
- Practice self-care consistently
- Address problems before they become crises
The hard truth? Society determines how fast you travel down the depression-to-pain highway.
Breaking the Cycle: What Actually Works

Okay, enough doom and gloom. Let’s talk solutions.
The revolutionary thing about this research? It gives us an 8-year window to do something about it.
Spot the Early Warning Signs
Think of depression as your body’s check engine light for future pain.
Watch for these red flags:
- Persistent sad mood lasting weeks
- Losing interest in things you used to enjoy
- Sleep is getting weird (too much or too little)
- Brain fog or trouble making decisions
- Feeling hopeless or worthless
- Pulling back from people
Don’t wait for it to get “bad enough.” Early intervention can prevent years of suffering.
The Treatment Revolution
The old approach was like trying to fix a leak by mopping the floor.
The new way? Treat your mind and body as the connected system they actually are.
What’s working now:
- Integrated care that addresses mental and physical symptoms together
- Anti-inflammatory treatments (yes, some antidepressants reduce inflammation)
- Movement therapy that helps both mood and pain
- Mindfulness practices that rewire pain perception
- Social connection programs that treat loneliness like the medical issue it is
Your Anti-Inflammation Toolkit
Anti-Inflammatory Arsenal
Science-backed tools to fight the inflammation cascade
Inflammation Reduction Potential
🥗 Food as Medicine
🐟 Omega-3 Powerhouses
🫐 Antioxidant Champions
🥬 Leafy Greens
💪 Movement That Heals
Walking
Strength Training
Yoga/Stretching
Swimming
🧠 Stress-Busting Strategies
Quick Relief (5-15 min)
Long-term Building
Implementation Timeline
Remember: Consistency beats perfection. Even small changes can reduce inflammation by 20-30% within 8 weeks.
Want to fight back against the inflammatory cascade before it starts?
Here’s your arsenal:
Food as Medicine
- Omega-3-rich fish (salmon, sardines, mackerel)
- Colorful vegetables packed with antioxidants
- Berries (nature’s anti-inflammatory powerhouses)
- Leafy greens (your brain’s best friends)
Movement That Heals
- Regular walking (even 20 minutes counts)
- Strength training (builds both muscle and mood)
- Yoga or stretching (reduces stress hormones)
- Any activity you actually enjoy (consistency beats intensity)
Stress-Busting Strategies
- Deep breathing (5 minutes can change your day)
- Quality sleep (7-9 hours, non-negotiable)
- Time in nature (even a houseplant helps)
- Limiting inflammatory foods (you know what they are)
Remember: You don’t have to be perfect. You just have to start somewhere.
Sarah’s Story: How Understanding Changes Everything

Let me tell you about Sarah, a 54-year-old teacher who lived through exactly what this research describes.
Three years after her divorce, when the worst of her depression seemed behind her, her body started falling apart. Lower back pain during her commute. Aching knees after short walks. Shoulders that felt like they carried invisible weights.
“The doctors kept telling me nothing was wrong,” Sarah recalls. “I’d leave feeling like I was making it all up.”
But once Sarah learned about the depression-pain connection, everything clicked. She found providers who treated both conditions together.
It took time, but the “mysterious” chronic pain that had seemed untreatable began to improve.
“I wish I had known eight years ago that my depression wasn’t just about my divorce,” she reflects. “Maybe I could have prevented some of this pain.”
The good news? Understanding this connection gave Sarah hope—and tools—to prevent things from getting worse.
What This Means for You Right Now

If you’re reading this and recognizing yourself in these patterns, here’s what I want you to know:
You’re not broken. You’re not imagining it. You’re experiencing a well-documented biological phenomenon.
Your Immediate Action Plan
If you’re dealing with depression or chronic stress right now:
- Take it seriously – it’s not just mental health, it’s whole-body health
- Don’t wait for pain to start – prevention is so much easier than treatment
- Find integrated care – look for providers who understand the mind-body connection
- Build one quality relationship – seriously, just one person who really gets you
- Start small with inflammation-fighting habits – pick one thing and stick with it
If you’re already dealing with both depression and pain:
- You can still improve – it’s never too late to break the cycle
- Seek integrated treatment – don’t let providers treat them separately
- Focus on what you can control – diet, movement, sleep, stress management
- Be patient with yourself – healing takes time, but it is possible
- Get support – you don’t have to figure this out alone
The Ripple Effect: Why This Matters Beyond You
Here’s something that might motivate you if personal benefit isn’t enough:
People with both depression and chronic pain have the highest rates of functional limitations in daily life.
When you address depression before it becomes pain, you’re not just saving yourself years of suffering. You’re preserving your ability to be there for the people who need you.
Your kids. Your partner. Your friends. Your work. Your community.
Taking care of your mental health today is an investment in the well-being of everyone who depends on you tomorrow.
The Bottom Line: Your Future Doesn’t Have to Hurt
The research is crystal clear: treatment for depression can prevent or reduce later physical pain.
Your mind isn’t separate from your body. It’s the architect of your physical future.
The question isn’t whether depression affects physical health anymore.
The question is: what are you going to do with this knowledge?
Your future self – the one eight years from now – is counting on the choices you make today.
The shadow of depression is long, but it’s not inevitable.
With the right tools, support, and understanding, you can step out of that shadow and into a future where both your mind and body can thrive.
Take Action Today: Your Next Steps

Ready to break the cycle before it starts? Here’s exactly what to do:
If You Need Help Right Now
- Call SAMHSA’s National Helpline: 1-800-662-HELP (4357) – free, confidential, 24/7
- Text HOME to 741741 for crisis text line support
- Talk to your doctor about integrated mental health care
If You Want to Prevent Problems
- Start a mood journal – track patterns before they become problems
- Find one stress-reduction technique you can do daily
- Schedule a mental health check-up just like you would a physical one
- Build stronger connections with people who matter to you
Share This Knowledge

- Send this article to someone who needs it – you might prevent years of their suffering
- Talk to your healthcare providers about the depression-pain connection
- Advocate for integrated care in your community
Your pain doesn’t have to be inevitable. Your future can be different.
But only if you start today.
What’s the one thing you’ll do differently after reading this? Drop a comment below – your story might be exactly what someone else needs to hear.






